What Causes Cervical Cancer?
Nearly all cervical cancer cases are caused by a virus called HPV (human papillomavirus). HPV infections are very common—most people who are sexually active will become infected at some point without ever knowing it.
There are many types of HPV:
- High-risk HPV types can infect cervical cells and cause cervical cancer. They can also infect other areas of the body and cause additional cancers.
- Low-risk HPV types can cause genital warts.
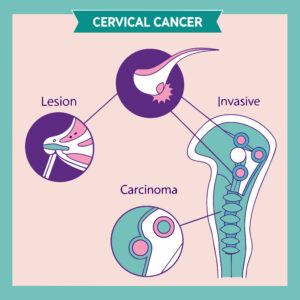
Most HPV infections go away on their own without causing any problems. However, some high-risk HPV infections do not clear naturally. When a high-risk HPV infection of cervical cells persists for many years, the cells can become abnormal. Over time, these changes may progress and develop into cervical cancer.
Why Is Screening Important?
Screening tests are used to check for disease before any symptoms appear. The goal of cervical cancer screening is to identify abnormal cells early—before they become cancerous—when treatment can effectively prevent cancer from developing.
Talk with your family and friends about the importance of cervical cancer screening. Each year, more than 4,000 women in the United States die from cervical cancer. Routine screening, along with early detection and treatment, can reduce the risk of developing cervical cancer by up to 90%.
Screening Recommendations
Ages 21–29:
- Get your first Pap test at age 21 and repeat every 3 years.
Ages 30–65: Choose one of the following options:
- HPV test every 5 years
- HPV/Pap cotest every 5 years
- Pap test every 3 years
Age 65 and older:
- Talk with your healthcare provider to determine if screening is still needed.
What If Screening Results Are Abnormal?
Most women with abnormal cervical screening results do not have cancer. However, it’s important to receive the recommended follow-up care. Next steps depend on your risk of developing severe cervical cell changes that could lead to cancer if untreated.
Your provider may recommend:
- A repeat HPV test or HPV/Pap cotest in 1 to 3 years
- A colposcopy and biopsy
- Treatment for abnormal cells
What Is a Colposcopy?
A colposcopy is a procedure that allows your healthcare provider to closely examine the cervix. During the procedure:
- A speculum is inserted to gently open the vagina.
- A vinegar solution is applied to highlight abnormal areas.
- A colposcope, a lighted magnifying instrument, is used to view the cervix in detail.
During a colposcopy, your provider may perform a biopsy—removing a small tissue sample from the cervix for examination under a microscope. Some women experience mild cramping, bleeding, or discharge afterward.
Biopsy samples are reviewed by a pathologist for Cervical Intraepithelial Neoplasia (CIN)—a term describing abnormal cells found on the surface of the cervix.
Treatment Procedures
LEEP (Loop Electrosurgical Excision Procedure):
A thin wire loop carrying an electrical current is used to remove abnormal tissue. Local anesthesia is applied to numb the area. The procedure takes only a few minutes and is performed in your provider’s office while you remain awake.
Cryotherapy:
A special cold probe is used to freeze and destroy abnormal tissue. This office procedure also takes only a few minutes and usually does not require anesthesia.
Other treatments may be necessary and can be arranged through a referral.
Interested in More Information?
Contact our Program Coordinator:
Ruth Brigantty
Office: (828) 404-3835
Cell: (980) 421-8496
Email: rbrigantty@kintegra.org